Best Practices for Sports Physicals
Potentially the only annual medical examination children and adolescents will receive, sports physicals are a great opportunity to provide a thorough evaluation.
Potentially the only annual medical examination children and adolescents will receive, sports physicals are a great opportunity to provide a thorough evaluation.
Summer is here, a season of backyard barbecues, splashing in the pool, summer camps, and family vacations. Before you know it, though, back-to-school time will be upon us. This means that retail clinics are ramping up for the scores of children needing medical clearance to play sports. It’s time to share and review best practices in the performance of sports physicals.
As health care providers, our primary objective is to screen for conditions that may be life-threatening or disabling, or that may predispose a patient to injury or illness.1Our goal is to facilitate safe participation, promote healthy behaviors, screen for risk factors, and educate on safety. A sports physical will be the only medical evaluation that approximately 30% to 88% of children and adolescents will receive each year.2Let’s use this opportunity to evaluate general health, discuss high risk behaviors, and encourage preventive care measures.
What Are Those Age Considerations Again?
Best Practice #1: When performing a sports physical, know the age considerations.
In children aged 6 to 10 years, focus on identifying any congenital abnormalities.3At this age, they are not competitive to win at all costs, they just want to play with their friends. By the ages of 11 to 15 years, patients are experiencing rapid physical growth and sexual maturation.3Intensive social development is a key factor. Take a minute to determine general health with anticipatory guidance. Encourage physical activity for health promotion, and be aware of the danger of drug abuse at this age. Between the ages of 16 to 30 years, the focus of the exam should depend on the type of sport being played.3It is important to identify earlier injuries, as these patients have probably been playing sports for several years. There is a high potential for narcotic abuse, and always a need for anticipatory guidance.
A History Lesson
Best Practice #2: Get a good history.
The medical history is where you will identify 90% of potential health issues that need to be taken into consideration.2The history form will prompt you to review questions regarding the use of medications, supplements, and substances used to increase strength and endurance, as well as drug abuse. Ask about all prescription and OTC medications as well. Children and adolescents are abusing OTC meds such as dextromethorphan, pain relievers, caffeine pills, pseudoephedrine, motion sickness pills, diet pills, laxatives, diuretics, and herbals.4Few teens and adults recognize the dangers of OTC meds, and studies have shown that those who learn about the risk of drugs at home are 50% less likely to abuse OTC drugs.4The point is to ask and educate parents and children about unhealthy habits. With adolescents, part of the sports physical should be performed without a parent or guardian present so that the clinician can inquire about risk-taking behavior.
The history also addresses mental health, eating disorders, and menstrual cycle disorders. Do a brief nutritional assessment and address concerns regarding overweight/obesity, and be sure to screen for eating disorders.2Identify any issues by asking questions about recent weight loss, eating habits, and body image in order to educate patients and get them the help they need. Obesity is an epidemic; children need physical activity!
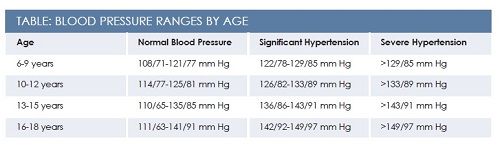
Think Beyond 110/70
Best Practice #3: Remember that abnormalities in blood pressure and visual acuity are commonly found during a sports physical.
The takeaway here is that even with significant hypertension, children can play sports as long as there is no indication of end‑organ disease.5Patients with severe hypertension should not be cleared until further evaluation has been completed, however. Know the appropriate ranges for blood pressure based on patient age (Table).5
For visual acuity, if significant visual impairment is present (20/50 acuity or worse) or a significant abnormality is identified, a complete ocular exam with dilated retinoscopy is warranted before clearance.2A patient with visual impairment of lesser severity can be cleared, with recommendations given for follow- up.
About That History & Physical
Best Practice #4: Be familiar with the 12 current American Heart Association recommendations for history and physical exam.6
During the personal history portion of the screening, ask patients about the following topics7:
(1) Exertional chest pain/discomfort
(2) Unexplained syncope/near-syncope
(3) Excessive exertional and unexplained dyspnea/fatigue with exercise
(4) Prior recognition of a heart murmur
(5) Elevated systemic blood pressure
When you ask about chest pain/ tightness/pressure with exercise, the differentials may be myocardial ischemia with exercise, congenital coronary artery anomalies, or left ventricular hypertrophy. More likely, however, exercise‑induced bronchoconstriction or gastroesophageal reflux disease is the culprit. If a patient answers affirmatively when asked if they’ve passed out/experienced syncope, the next question to ask is, “When did you pass out? Was it during exercise or after exercise?” If the answer is “during,” that’s a red flag for cardiovascular disease. If the answer is “after,” then it’s most likely a vasovagal episode, and if the episode was accompanied by loss of consciousness, a workup is warranted. Clinicians are directed to ask about unexplained dyspnea and fatigue because these symptoms could indicate myocarditis or hypertrophic cardiomyopathy.
A patient who has experienced skipped heartbeats or palpitations may have an arrhythmia, supraventricular tachycardia, or Wolff-Parkinson-White syndrome, and may need further investigation before clearance. Ask about prior cardiac testing; any history of testing should be investigated fully with review of past medical records before clearance. Family history topics to inquire about include7:
(6) Premature death of a relative before age 50 due to heart disease
(7) Disability from heart disease in a close relative aged 50 years
(8) Specific knowledge of certain cardiac conditions in family members: hypertrophic or dilated cardiomyopathy, long-QT syndrome or other ion channelopathies, Marfan syndrome, or clinically important arrhythmias
If there is a family history of any of the above, recommend that the patient follow up with a cardiologist for evaluation. The AHA also recommends that the following steps be taken during a cardiac exam7:
(9) Listen for a heart murmur
(10) Palpate femoral pulses simultaneously with radial pulses
(11) Check for the physical stigmata of Marfan syndrome
(12) Obtain brachial artery blood pressure (while sitting)
Listen to the Heart
Best Practice #5: Know what to do with a heart murmur.
There is a good chance that you will see a child with a history of a heart murmur, a known heart murmur, or a family history of cardiac disease, or that you will identify a new murmur during an exam. What if the murmur you hear is a soft early systolic murmur grade 1 or 2? What if the murmur is mid-systolic and vibratory or musical (a Still’s murmur)? Both of these types of murmurs are likely innocent, and in the absence of concerning symptoms or family history, no further investigation is needed. Always auscultate the heart while the patient is supine and standing. The diagnostic murmur of hypertrophic cardiomyopathy becomes louder with standing. When you hear a murmur, remember to perform a maneuver to potentially amplify a systolic murmur.
Best Practice #6: Recognize causes of sudden cardiac death and signs of Marfan syndrome.During sports, 90% of sudden cardiac deaths occurred in male African-American high school patients.2The most common cause is hypertrophic cardiomyopathy.8Other causes are congenital coronary anomalies like the anomalous origin of left main coronary artery from right sinus of valsalva or cystic necrosis of the tunica media of the aorta causing rupture, most commonly seen in Marfan syndrome.8
Abnormal vital signs may be an indication to withhold clearance pending further evaluation. Patients with a heart rate over 120 beats per minute, severe hypertension, or history of arrhythmias should be referred for further evaluation. Be sure to also check for radial and femoral pulse wave abnormalities in both extremities. If delayed, think aortic coarctation and refer the patient to a cardiologist. Again, listen for a heart murmur with the patient standing and supine.
Refer patients with the following for further evaluation2:
• Any systolic murmur grade 3 through 6 or louder
• Any murmur that disrupts normal heart sounds
• Any diastolic murmur
• Any murmur that intensifies with maneuvers/changes in the patient’s position
Look for the following characteristics to identify patient’s with Marfan syndrome5:
• Arm span longer than standing height
• Severe scoliosis
• Concave chest deformity
• Positive thumb and/or wrist sign
• High arched palate
• Hyperextensible joints
• Pes planus
• Murmurs of aortic or mitral regurgitation or prolapse
If you find any of these abnormalities, postpone sports clearance until the patient goes for further evaluation. Ninety percent of deaths in patients with Marfan syndrome were attributed to rupture of an aortic aneurysm, aortic dissection, and severe aortic insufficiency.3Children who may have Marfan syndrome need a referral to a cardiologist for electrocardiogram and echocardiogram.
More Than Just a Bump on the Head
Best Practice #7: Be confident in clearing or referring your patient with history of a concussion.Approximately 300,000 concussions occur each year in the United States.2Concussion education should be included at every sports physical. A history of a concussion puts the patient at higher risk for future concussion, and multiple concussions can lead to long‑term sequelae.2Ask about and document symptom resolution, and do a neurological exam. In post-concussion syndrome, symptoms such as headache, dizziness, and fatigue can persist for weeks to years.2Look for persistent neurological deficits, and remember that depression can be caused by repetitive concussions. Inquire about second-impact syndrome, which occurs when a second concussion takes place before the first concussion has resolved. Do not clear post-concussion syndrome, persistent neurological deficits, or second-impact syndrome until the patient has been seen by a neurologist.
Once these 3 conditions above are ruled out, use these guidelines to determine need for follow-up2:
• A patient who has sustained 2 or 3 concussions without loss of consciousness should be referred for evaluation.
• A patient who has sustained 1 or 2 concussions with loss of consciousness should be referred for further evaluation.
• A patient who has sustained 3 or more concussions or delayed recovery should be considered for temporary or permanent disqualification from contact sports, but that decision will be made by the neurologist.
Ever Broken a Bone?
Best Practice #8: Know how to examine a child with a history of a sprain, fracture, or dislocation.
Musculoskeletal findings are the most common cause of restriction from sports.2Accurate history detects more than 90% of them.2Inquire about previous injuries and perform an examination of affected areas. If there is a history of injury, assess that specific area for signs of2:
• Joint effusion
• Abnormal range of motion or ligament instability
• Less than 80% to 90% of strength in the affected extremity
If any of these are present, further evaluation is needed prior to clearance. Clearance is based on degree/type of injury and the requirements of the sport.2If the sport will not affect the injured area, the patient can be cleared. Consider education on padding, taping, bracing, and strength/conditioning exercises.
A previous injury is a major risk factor for reinjury. Inquire about the course of treatment for injury and if rehabilitation was indicated. If you are uncertain of a patient’s ability to participate due to previous injury, refer that patient to the clinician who initiated treatment for the injury for reevaluation and determination of clearance.
Take a Deep Breath
Best Practice #9: Understand exercise- induced bronchoconstriction and asthma, and know what questions to ask.
The term “exercise induced asthma” has now been replaced by “exercise induced bronchoconstriction” (EIB). EIB is used to describe the transient and reversible narrowing of the lower airways that follows vigorous exercise, and it can occur in patients who do not have asthma.9EIB is found in 8% to 10% of healthy school-age children and in 35% of children with asthma.9Highly increased ventilation and the inhalation of cold, dry air; air pollutants; and chlorine are thought to be important triggers of EIB. Signs and symptoms include cough, wheezing, chest tightness, dyspnea, and excess mucous production.2The prevalence of EIB is reported to be up to 40% in patients with allergic rhinitis.9
It is important to identify which medications a patient with asthma is taking. Note how frequently the rescue inhaler is used. If asthma is controlled and the patient is active, no further work-up is needed; written action plan is highly recommended, however. Educate the child and parent to use a quick‑relief inhaler 15 minutes prior to game time and to keep an inhaler with them during participation. Perform peak flow meter daily, as well. This can help identify when further evaluation and treatment may be needed. Early recognition of exacerbation with appropriate stepping up of medication is important.1
Physical activity is beneficial for young patients with asthma. When asthmatic symptoms are well controlled, most patients are able to perform without restriction.
A Note About Sickle Cell
Best Practice #10: Know how to educate a patient with sickle cell trait or disease.
If a child has a family history of sickle cell disease or the trait for it, it is recommended that they obtain confirmatory testing. Currently, the only athletes required to undergo screening for sickle cell are those participating in NCAA Division I sports.10Patients who have sickle cell disease may still be cleared for participation in sports after individual assessment.11
Patients with the sickle cell trait are symptom-free carriers of the disease and are typically not at increased risk. However, for both the trait and disease, risk can be increased when high-exertion activity is performed under extreme conditions of heat and humidity or increased altitude. Here are key points to educate the parent and patient with sickle cell trait on or about disease10:
• Progressive conditioning to the environment and to the intensity and duration of activities is necessary. Heat stress and dehydration with intense physical exertion can exacerbate the onset of sickling.
• The athlete must sufficiently hydrate to reduce the risk of exertional heat illness and/or rhabdomyolysis, and take frequent rest and recovery periods.
• Watch for muscle cramping, pain, swelling, weakness, tenderness, and shortness of breath. If any of these occur, stop the activity and err on the side of caution.
As we head into back-to-school season, our goals are to provide high-quality care in the identification of life-threatening conditions and to minimize cardiovascular risk associated with sports participation. The sports physical is an opportunity to promote a lifelong habit of physical activity and to advocate for sports participation.
Kristen Marjama, DNP, MSN, FNP-BC, is a board certified family nurse practitioner with 17 years of healthcare experience. She began her career as a Registered Nurse in traumatic brain injury rehabilitation, emergency medicine, and the cardiac catheterization lab. As a Nurse Practitioner, she worked in private family practice before accepting a position in the retail health care clinic setting in 2008. Her passion is for the provision of high quality care that is according to evidence-based guidelines.
References
1. Sanders B, Blackburn TA, Boucher B. Preparticipation screening—the sports physical therapy perspective.Int J Sports Phys Ther. 2013;8(2);180-193.
2. Conley KM, Bolin DJ, Carek PJ, Konin JG, Neal TL, Violette D. National Athletic Trainers' Association position statement: preparticipation physical examinations and disqualifying conditions.J Athl Train. 2014;49(1):102-120. doi: 10.4085/1062-6050-48.6.05.
3. Mujovic VM, Cubrilo DG. Pre-participation sports screening.Phys Cult. 2012;66(2),138-146.
4. Cohen MR. 10 over-the-counter medicines abused by teens.The Philadelphia Inquirer. October 17, 2013.
5. Womack J. Give your sports physicals a performance boost.J Fam Pract. 2010;59(8):437-444.
6. Morse E, Funk M. Preparticipation screening and prevention of sudden cardiac death in athletes: implications for primary care.J Am Acad Nurse Pract. 2012:24(2);63-69. doi:10.1111/j.1745-7599.2011.00694.x
7. Mahmood S, Lim L, Akram Y, Alford-Morales S, Sherin K; ACPM Prevention Practice Committee. . Screening for sudden cardiac death before participation in high school and collegiate sports: American College of Preventive Medicine position statement on preventive practice.Am J Prev Med. 2013:45(1):130-133. doi: 10.1016/j.amepre.2013.04.002.
8. Badwal KK. Pre-participation examination: tool for cardiovascular screening of competitive athletes.Sport Sci Rev. 2013;22(5); 405-415. doi: 10.2478/ssr-2013-0020
9. Wuestenfeld JC, Wolfarth B. Special considerations for adolescent athletic and asthmatic patients.Open Access J Sports Med. 2013;4:1-7. doi: 10.2147/OAJSM.S23438.
10. Jones J. Sickle cell trait in sports.Hughston Health Alert. 2011;23(3):4-5.
11. Medical conditions that may rule out sports participation. American Academy of Pediatrics website. www.healthychildren.org/English/health-issues/injuries-emergencies/sports-injuries/Pages/Medical-Conditions-That-May-Rule-Out-Sports-Participation.aspx. Updated May 5, 2015.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.
