Written Asthma Action Plan
The National Health Interview Survey in 2014 estimated that 17.7 million adults and 6.3 million children had asthma.
The National Health Interview Survey in 2014 estimated that 17.7 million adults and 6.3 million children had asthma.1How are we doing with educating patients on managing asthma? An educated patient is an important key to controlling asthma nationwide. It is important to manage this chronic disease with regularly scheduled follow-up visits, shared decision making, monitoring of quick-relief medication use, and continuing asthma education. Moreover, a written asthma action plan (WAAP) is recommended for every patient with asthma.2
Because asthma is a chronic disease with intermittent worsening of symptoms, medication adherence plays an important role in maintaining asthma control and managing these worsening symptoms. Even though study results have shown that WAAPs contribute to improved asthma medication adherence, evidence suggests that as few as 25% of eligible patients have one.3Fewer than 1 in 2 children and 1 in 3 adults are likely to receive a WAAP,4which means that health care providers can have a major impact on helping pa- tients take control of their asthma by making asthma education a priority and utilizing a WAAP.
Children are more likely than adults to learn how to manage their asthma. More than 8 in 10 children, but fewer than 7 in 10 adults, are taught how to recognize asthma symptoms.4Health care providers should keep in mind that not all patients know how to recognize asthma. Therefore, education is essential, and an individualized WAAP can be created to serve 2 main purposes. First, the WAAP is used to inform the patient (or parent/caregiver) how to maintain daily asthma symptom control.2This includes outlining the steps the patient must take to keep asthma from worsening. Second, it provides guidance to help the patient know when and how to treat worsening symptoms.2
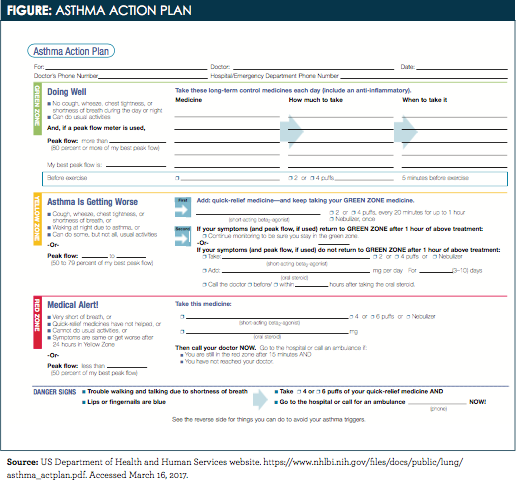
WAAPs can take varying forms, but the goal should be to use the one that works best for the patient and is easiest for the health care provider to create. WAAPs can either be printed out and then filled in, or some can be completed online before printing; computer-based programs can also help create 5 individualized WAAPs. WAAPs are typically divided into 3 different color zones: green (no symptoms), yellow (having symptoms), and red (having symptoms that aren’t responding to a quick relief medication).
In general, an effective WAAP must contain the following information6:
- Patient’s treatment options: long-term control and quick-relief medications with instructions
- Potential precipitating factors and asthma triggers to avoid (if applicable)
- What signs and symptoms (or peak flow measurements) indicate worsening asthma
- Action points: when, what, and how to take a medication for how long and what to expect
- When to seek immediate medical care: Signs of severe exacerbations
- Phone numbers for an emergency contact, health care provider, and local hospital
TheFigureis an example of a WAAP7.
The primary focus of the WAAP can be found in the action points. Patients require education about their medications. Asthma medications can be categorized into 2 classes: long-term control medications and quick-relief medications. Quick-relief medications, such as short-acting beta agonists, are used to treat symptoms and exacerbations. Long-term control medications are used to achieve and maintain control, such as inhaled corticosteroids and long-acting beta agonists. Here are some key education tips for each of these classes of medication.
Short-acting beta agonists6:
- Use when short of breath; with cough, chest tightness, or wheezing; or if your peak expiratory flow decreases 10% to 20% from the baseline.
- List the quick-relief medication name with directions, such as 2 puffs every 4 to 6 hours. Or if severe, consider recommending 2 puffs every 5 minutes up to 20 puffs. If no response in 1 hour, the patient needs to seek immediate medical attention.
- It is important for the patient to understand WHY the increased need for the quick relief medication is a red flag and should be reported to the health care provider.
Long-acting beta agonists6:
- This is not a quick-relief medication, but it helps to reduce exacerbations and can also help to keep patients on a lower dose of the ICS. Dosing typically does not change during an exacerbation, but additional studies are needed to clarify this practice
- It is typically used along with an ICS and can also be ordered in combination formulations.
- List the medication name with directions accordingly.
Although WAAPs are useful for everyone with asthma, they are particularly important for those who have moderate or severe persistent asthma, a history of severe exacerbations, or poorly controlled asthma. In addition to understanding what the WAAP should contain, it is also helpful to look at the factors that may contribute to the low rate of use or misuse of the WAAP. A study revealed that patients indicated the following reasons for underuse3:
- The health care provider never offered them a WAAP.
- The patient did not feel confident about using the WAAP, or did not use it at all.
- The patient did not understand the WAAP.
- The patient did not feel that the health care provider believed the WAAP would be effective for self-management.
What can we do to combat these factors? It is not hard to offer a patient of WAAP, yet it does require time and individualization. To help the patient feel confident about using the WAAP, it is important to encourage patient participation in the development of the plan. This will help to ensure the plan is created at the patient’s level of understanding. Health literacy is a common theme in the literature. A need exists for communication in plain language due to barriers for patients with poor health literacy skills. From this perspective, the action plan needs to be written so that it is easily understood by the adult patient, child, or parent/caregiver.
Do we as health care providers believe that the WAAP is an effective tool in empowering patients for self-management? We can demonstrate our belief by asking about and reviewing the WAAP at each visit. For each patient who comes in with a history of asthma, we should be asking if they have a WAAP. Inquire if the patient has any questions about the plan. If patients are being asked these questions at each visit, they are going to get the idea that it’s important! Asking about the WAAP also helps health care providers to gain a better understanding as to how well the patient can identify their own asthma control. It is also an opportunity to identify patient concerns that can be addressed to improve upon their individual self-management strategy. An educated patient can slow the progression of asthma and improve outcomes in our communities.
Kristen Marjama, DNP, FNP-BCis a doctorally prepared family nurse practitioner with 9 years of experience in the retail health care clinic industry. Dr Marjama is the Manager of Clinic Education and Profes- sional Development at Walmart Care Clinic.Her passion is for the provision of high-quality care with a primary focus on educationof evidence-based guidelines. She enjoys speaking at conferences, networking with health care professionals, and was selected this year to participate in the Leadership Program through the American Association of Nurse Practitioners (AANP).
References
- National Center for Health Statistics. Asthma. CDC website. www.cdc.gov/nchs/fastats/asthma.htm. Updated January 19, 2017. Accessed February 23, 2017.
- Asthma Action Plan. CDC website. www.cdc.gov/asthma/actionplan.html. Updated February 14, 2012. Accessed February 23, 2017.
- Andrews KL, Jones SC, Mullan J. Asthma self-management in adults: a review of current literature.Collegian.2014;21(1):33-41. doi: 10.1016/j.colegn.2012.12.005.
- National Heart, Lung, and Blood Institute. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Department of Health and Human Services; National Institutes of Health website. www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines/full-report. Published August 28, 2007. Updated April 2012. Accessed June 5, 2015.
- Tools for Asthma Control. CDC website. cdc.gov/asthma/tools_for_control.htm. Updated February 27, 2012. Accessed February 24, 2017.
- Rank MA, Volcheck GW, Li JT, Patel AM, Lim KG. Formulating an effective and efficient written asthma action plan.Mayo Clin Proc.2008;83(11):1263-1270. doi: 10.4065/83.11.1263.
- National Heart, Lung, and Blood Institute. Lung Diseases. Asthma Action Plan. Department of Health and Human Services; National Institutes of Health website. www.nhlbi.nih.gov/health/resources/lung. Accessed February 24, 2017.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.
