10 Steps to Counseling Patients With Rosacea
Retail health care practitioners can treat patients with rosacea in 10 easy steps.
Rosacea, an incurable chronic condition, affects more than 16 million Americans and usually presents in adulthood.1Common signs include central facial erythema, flushing, and inflammatory lesions (papules, pustules). Rosacea has inflammatory, neural, and vascular components.2
Retail health care practitioners can treat patients with rosacea in these 10 easy steps:
1. Set realistic expectations.Researchers have not identified rosacea’s underlying cause. Symptom frequency and severity are patient specific and can vary over time. Successful symptom management involves avoiding triggers, using gentle skin care products, and, often, prescription medication.3
2. Raise resource and support system awareness.Most patients with rosacea experience depression, embarrassment, social anxiety, and stress. Emotional stress can trigger outbreaks, creating a cycle detrimental to mental health.4Cognitive behavioral therapy relieves anxiety, a fear of blushing, and stress.5Social support forums and groups also help patients with rosacea manage the psychological effects. Table 1 lists patient-friendly resources.
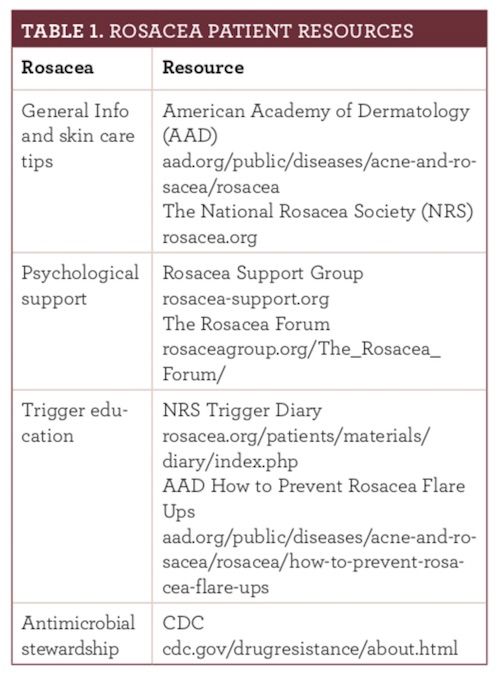
3.Identify specific triggers.Recognizing triggers (see Figure 16) is essential to avoid exacerbation. Sun exposure is the most common trigger, so advise patients to wear protective clothing and sunscreen every day.7Long-term topical beta-blockers, corticosteroids, niacin, and vasodilator scan also trigger flare-ups.8
Recommend that patients keep a diary or take daily selfies, noting what activities, diet, and exposures contribute to symptom exacerbations. The National Rosacea Society offers a free trigger diary (rosacea.org).6
4. Stress behavior modifications, especially sun avoidance.Sun exposure can worsen rosacea even in those with dark skin, so all patients must wear sunscreen year round. Recommend broad-spectrum sunscreen with a sun protection factor of 30+ and ingredients that reflect ultraviolet rays, such as titanium oxide and zinc oxide.9
Patients should avoid physical activities (bike riding, football, horseback riding, etc) that cause facial friction or require headgear. Although they need to remove facial dirt and oil, patients also must limit showering to once or twice daily with lukewarm water and mild cleansers. Immediately after showering, they can apply unscented emollients or oils.10
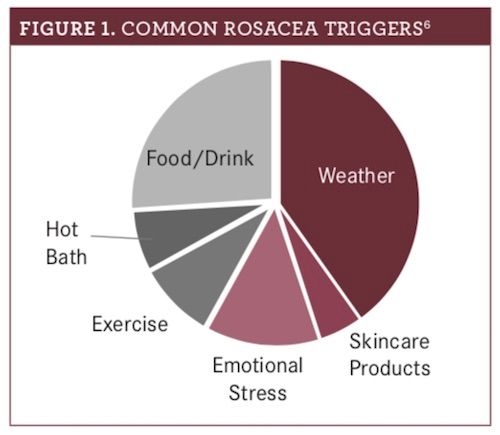
5. Determine the patient’s top treatment priority.Most topical rosacea treatments are available in various forms (see Figure 211,12).11Ask patients what features they dislike or like to improve adherence. Ask what they have tried in the past, recommending OTC products first and then prescribing if necessary. Undertreatment is common, so do not shy away from prescription products.12
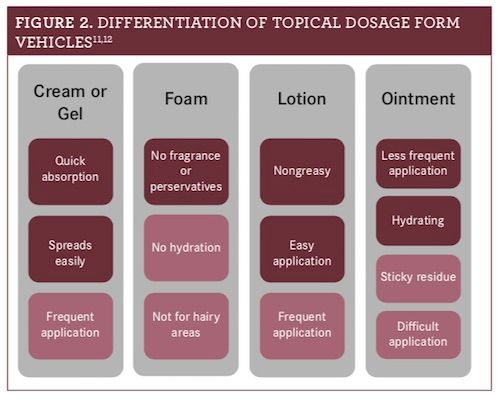
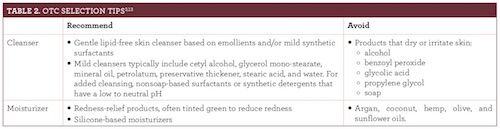
Table 23,13describes OTC product characteristics.
7. Offer an everyday facial skin care routine example, such as this one3,9,11:
- Cleanser.Cleanse first, massaging with fingertips in a circular motion, and avoid abrasive cloths or tools. Rinse the cleanser off and gently pat dry.
- Medication (if applicable). Apply products with the thin- nest consistency before occlusive ointment-based products.11Refer to package inserts for medication-specific application instructions.
- Moisturizer.Wait a few minutes until medication completely dries before gently applying moisturizer.
- Sunscreen.For the greatest barrier protection, apply sunscreen to dry skin.
- Make-up (if applicable).Use light liquid-based foundation that spreads easily. Avoid difficult-to-spread-and-remove foundations and waterproof makeup.9
8. Manage expectations for topical prescriptions.Select prescription topicals based on patient-specific subtypes and most bothersome symptoms. Azelaic acid and metronidazole address papulopustular lesions. Common adverse effects include burning, itching, skin irritation, and stinging. This regimen takes at least 6 to 8 weeks for a therapeutic response; azelaic acid is slightly more rapid acting.2Advise patients that they will use topical agents for life.7
Brimonidine gel lessens persistent bothersome redness between flare-ups within 30 to 60 minutes. Rebound or worsening redness is a potential adverse effect, along with burning, contact dermatitis, and flushing. Assess efficacy in 2 to 4 weeks.2
9. Consider oral anti-inflammatory antibiotics. Patients with moderate to severe rosacea can take an anti-inflammatory dose of modified-release doxycycline in addition to, or instead of, topical therapies. For flare-ups, use doxycycline (40 mg/d) for 10 to 14 days and up to 9 months for maintenance. Reserve oral antibiotic doses of doxycycline (50 to 200 mg/d) for poor responders to low- dose antibiotic and topical regimens.2Inform patients that antibiotics for rosacea will not treat bacterial infections and cannot be used during pregnancy. Doxycycline can cause adverse gastrointestinal effects and sun sensitivity.14
10. Step-up treatment for refractory/severe cases.Isotretinoin is an option for refractory/severe cases, but it is contraindicated during pregnancy and requires frequent lab monitoring.2Some patients may opt for modalities such as laser light treatment, but the cost limits its accessibility.15Inform patients interested in complementary or alternative medicine options about the limited efficacy, and recommend sticking with FDA-approved products.13
Sara E. Milleris a PharmD candidate at the University of Connecticut School of Pharmacy in Storrs.
References
- What is rosacea? National Rosacea Society website. rosacea.org. Accessed June 27, 2018.
- Rosacea medical management guidelines. American Acne & Rosacea Society website. acneandrosacea.org/medical-professionals/rosacea-medical-management-guidelines. Accessed June 27, 2018.
- Del Rosso JQ, Baum EW. Comprehensive medical management of rosacea: an interim study report and literature review.J Clin Aesthet Dermatol. 2008;1(1):20-25.
- Survey shows controlling stress can reduce flare-up frequency. National Rosacea Society website. rosacea.org/rr/2011/fall/article_3.php. Published Fall 2011. Accessed June 27, 2018
- Heisig M, Reich A. Psychological aspects of rosacea with a focus on anxiety and depression.Clin Cosmet Investig Derm. 2018;11:103-107. doi: 10.2147/CCID.S126850.
- Coping with rosacea. National Rosacea Society website. rosacea.org/patients/materials/coping/intro.php. Accessed June 27, 2018.
- Rosacea diary booklet. National Rosacea Society website. rosacea.org/patients/materials/diary/index.php. Accessed June 27,2018.
- Litt JZ. Steroid-induced rosacea.Am Fam Physician. 1993;48(1):67-71.
- 6 rosacea skin care tips dermatologists give their patients. American Academy of Dermatology website. aad.org/public/diseases/acne-and-rosacea/rosacea/6-rosacea-skin-care-tips-dermatologists-give-their-patients. Accessed June 27, 2018.
- Subramanyan K. Role of mild cleansing in the management of patient skin. Dermatol Ther. 2004;17(suppl 1):26-34.
- Ballington DA, Anderson RJ.Principles of Pharmacy Practice. 5th ed.New Gloucester, ME: Medtech; 2014:59.
- Wehausen B, Hill DE, Feldmen SR. Most people with psoriasis or rosacea are not being treated: a large population study.Dermatol Online J.2016;22(7).
- Draelos ZD. Cosmeceuticals for rosacea.Clin Dermatol.2017;35(2):213-217. doi: 10.1016/j.clindermatol.2016.10.017.
- Oracea (doxycycline) [prescribing information]. Fort Worth, TX: Galderma Laboratories LP; 2013. www.accessdata.fda.gov/drugsatfda_docs/label/2013/050805s008lbl.pdf. Accessed July 5, 2018.
- Weinkle AP, Doktor V, Emer J. Update on the management of rosacea.Clin Cosmet Investig Dermatol.2015;8:159-177. doi: 10.2147/CCID.S58940.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.