Skin Care Has Key Role in Managing Diabetes
Health care professionals can play an important role in counseling patients on prevention and treatment strategies for skin conditions.
About 33% of individuals with diabetes will develop a skin disorder at some point.1A skin problem is generally a sign that blood glucose levels are too high. The good news is that many skin conditions can be prevented or easily treated when caught early. Health care professionals can play an important role in counseling patients on prevention and treatment strategies for skin conditions.
Diabetic Skin Conditions
Bacterial infections can occur in patients with diabetes and may include boils, folliculitis (hair follicle infection), or styes, which may need to be treated with antibiotics.2Fungal infections, especially Candida albicans, can also develop in warm moist skin folds. Antifungal medications, such as clotrimazole, miconazole, or nystatin, are generally used to treat Candida infections. Other common fungal infections that may occur in patients with diabetes include athlete’s foot, jock itch, ringworm, and vaginal infections. Clotrimazole can be used to treat these conditions, and miconazole can be used specifically for vaginal yeast infections. Patients may also experience localized itching caused by dry skin, poor circulation, or a yeast infection. Recommend that patients use a mild soap with moisturizer and apply skin cream after bathing.2
Acanthosis nigricans is a skin condition characterized by brown or tan raised areas that appear on the sides of the neck, armpits, and groin in overweight individuals.2Weight loss is the best treatment. Diabetic blisters can occur in patients with uncontrolled diabetes and those with diabetic neuropathy. The blisters generally appear on the backs of fingers, hands, toes, feet, legs, and forearms. Lowering blood glucose levels can help manage this condition. Eruptive xanthomatosis is caused by uncontrolled blood glucose levels, and it is characterized by firm, pea-like, yellow enlargements in the skin. The bumps have a red halo that may also itch, and they generally occur on the backs of hands, feet, arms, legs, and the buttocks. This condition usually occurs in young men with type 1 diabetes, and patients generally have high cholesterol levels. Lowering blood glucose levels is the best way to manage eruptive xanthomatosis.2
Preventing Skin Complications
Prevention is key when it comes to skin conditions in patients with diabetes. It is important to keep their diabetes well managed, because high blood glucose levels can lead to dry skin and an increased risk of infection.1 Advise patients to avoid bubble baths, hot baths, and showers if their skin is dry. Lotion can be applied to the skin but not between the toes, which will prevent fungal growth. It is important to avoid scratching dry or itchy skin, as this can cause an infection. Treat cuts immediately by washing with soap and water; an antibiotic cream or ointment can be applied after. Refer patients to a dermatologist if OTC products do not help.1
Foot Ulcer Prevention and Treatment
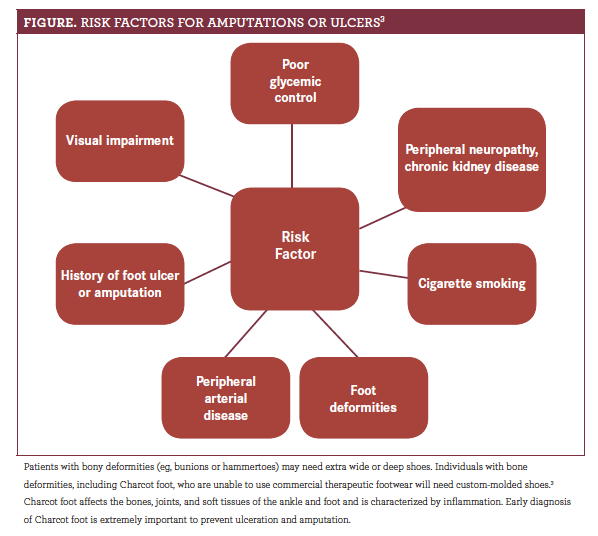
Educate patients about the importance of foot care and to check every day for cuts and sores.1 The American Diabetes Association recommends that individuals have a comprehensive foot evaluation at least annually to check for risk factors for amputations (figure).3
About 9 million to 26 million individuals with diabetes develop foot ulcers each year,4 and they should be seen by a podiatrist. Unfortunately, ulcer recurrence is common, with an estimated 40% experiencing another foot ulcer within a year after healing.4Early signs of skin damage to watch for that may be risk factors for ulcer recurrence include blistering, calluses, or hemorrhage.4Treatment of ulcers generally includes daily saline and dressings, debridement, and antibiotic therapy (soft tissue or bone infection).3Hyperbaric oxygen therapy has mixed evidence as an adjunctive treatment, as some study results did not show a benefit and the studies were not well designed.3Health care providers should educate about the appropriate footwear options for high-risk patients, which include the following:
- Broad and square toe box
- Custom therapeutic footwear
- Laces with 3 or 4 eyes per side
- Padded tongue
- Quality lightweight materials
- Sufficient size to accommodate a cushioned insole
Jennifer Gershman, PharmD, CPh, is a drug information pharmacist and Contemporary Clinic® contributor who resides in south Florida.
References
- Skin care. ADA. diabetes.org/living-with-diabetes/complications/skin-care.html. Updated May 10, 2016. Accessed February 10, 2019.
- Skin complications. ADA website. diabetes.org/living-with-diabetes/complications/skin-complications.html. Updated March 31, 2014. Accessed February 10, 2019.
- American Diabetes Association. 11. Microvascular complications and foot care: Standards of Medical Care in Diabetes-2019.Diabetes Care. 2019;42(suppl 1):S124-S138. doi: 10.2337/dc19-S011.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence.N Engl J Med. 2017;376(24):2367- 2375. doi: 10.1056/NEJMra1615439.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.