Allergic Rhinitis: Treatment and Management
One of the most common diagnoses in the United States, allergic rhinitis is often misdiagnosed and/or undertreated.
One of the most common diagnoses in the United States, allergic rhinitis is often misdiagnosed and/or undertreated.
Allergic rhinitis (AR) is one of the most common diagnoses in the United States, affecting an estimated 10% to 30% of adults and up to 40% of children.1Research estimates that AR is the reason for 13 million medical office visits annually,2many of which are to retail clinics. Each year, 25% of US households have at least 1 member with AR symptoms.3It is common for patients to have tried multiple OTC allergy medicines before they seek professional medical care for their AR symptoms. The financial and societal burdens of AR are significant and have been referred to by some as “massive.”4Studies show AR also has a negative impact on a patient’s quality of life, affecting emotional function, activities, sleep, and comorbid conditions.5
In 2006, a landmark study, “Allergies in America,” surveyed 2500 adults who had been diagnosed with either AR or nonallergic rhinitis and who had taken prescription allergy medication in the previous 12 months. The survey results demonstrated the most commonly reported symptom was nasal congestion. Nearly 40% of patients said that their related discomfort was intolerable without some sort of relief measures. Survey results also demonstrated an average productivity decline of 25% among employees on days when they had significant allergy symptoms and 30% of employees losing workdays due to uncontrolled allergy symptoms in the past year.5
AR is often misdiagnosed and/ or undertreated.3Patients with AR often present to medical practitioners requesting antibiotics for what they think is a sinus infection when what they need is appropriate treatment for AR. The misdiagnosis of AR contributes to and perpetuates the overuse of oral antibiotics. Retail clinic nurse practitioners (NPs) and physician assistants (PAs) are at the front line of patient care and have a great opportunity to educate patients regarding the commonality and characteristics of AR and offer an evidence-based treatment plan.
This article will review a case study of a patient with AR. The diagnosis and management of AR will be discussed along with evidence-based options for treatment.
History
Brooke is a 16-year-old girl, accompanied by her father, who presents to your clinic for the first time with the chief complaint of a flare of her allergy symptoms this fall. She states that since her school year started 2 months ago in early August, her “allergies have been terrible.” Brooke has had seasonal allergies since she was 9 years old, and her father states that they have typically controlled Brooke’s symptoms over the past several years with OTC antihistamines and OTC eye drops. He states that he typically sees a spike in Brooke’s allergy symptoms each spring when the trees start blooming, but that her symptoms are much better by July. Brooke reports having difficulty staying awake during her school day, and she is not sure if it is due to the allergy pill she takes in the morning or because her nasal congestion is keeping her awake at night. She is complaining of sneezing, an itchy nose, itchy eyes, clear runny nose, and postnasal drip. Brooke’s father states that the last time she had similar symptoms she was prescribed a 5-day course of antibiotics and wonders if she is getting more antibiotics today.
Brooke recently tried an OTC corticosteroid (fluticasone propionate) nasal spray after she and her father saw a poster about the medicine at her pharmacy. Typically, she only uses her nasal spray when her symptoms are “really bad,” but her current symptoms necessitated her using the nasal spray twice daily for the past 6 weeks. She states she doesn’t like nasal sprays very much because the medication “runs down” the back of her throat. She recently added a second-generation oral antihistamine to her daily medications, but her symptoms persist. She has also tried OTC allergy eye drops as needed and reports her eye symptoms have somewhat improved. When questioned, Brooke states she is adherent with her medications.
DISCUSSION QUESTION: What additional information would you want to know about Brooke’s history and current illness?
ANSWER:A patient’s medical history is critical to an accurate diagnosis. You decide that you need a more detailed medical history from Brooke and proceed to ask her additional questions that elicit the following information:
- Review of symptoms:Brooke complains of sneezing, and itchy nose, itchy eyes, clear runny nose, and postnasal drip. She denies any discolored nasal mucus, fever, sore throat, or headaches, and does not have coughing, shortness of breath, or nocturnal cough.
- Previous medical history:Brooke has no history of other medical problems or known drug allergies.
- Environmental history:Brooke and her family live in the Midwest in a home surrounded by trees on 1 acre of land. She has no pets, although she wants to adopt a cat. No one smokes around her. She redecorated her bedroom last year and, at that time, got a new mattress and pillow.
- Family history:Brooke’s mother has similar seasonal allergy symptoms that she treats with alternating OTC loratadine and cetirizine.
- Social history:Brooke is in 11th grade and has always been an excellent student; this school year, however, she has gotten off to a rough academic start. She is in choir and on the debate team, and her nasal congestion and postnasal drip have impacted her voice and ability to sing. She has upcoming tryouts for show choir, and it is very important that she is able to sing to the best of her ability.
DISCUSSION QUESTION: What is your initial impression of Brooke’s presentation?
ANSWER:Based on her history, you initially suspect AR. Brooke’s father again asks if she will be prescribed an antibiotic for treatment. You share that without evidence (on exam and/ or radiological imaging) of Brooke having a bacterial infection, there is no indication for antibiotics and that if antibiotics were prescribed in such a scenario, they wouldn’t be beneficial for symptom relief. Brooke’s father is satisfied with your answer. You then move on to Brooke’s physical exam and find the following:
- Physical exam:She is a well-developed, well-nourished teenager who has been sneezing periodically and appears congested. Allergic shiners present bilaterally.
- Vital signs:Normal. Weight = 140 lb; height = 68 in.
- Tympanic membranes:Normal bilaterally.
- Nose: Mucosa is pale and boggy with acutely edematous inferior nasal turbinates; clear rhinorrhea present. Nasal crease noted.
- Skin: No rashes.
- Chest: Bilateral breath sounds are clear to auscultation. No wheezing, rhonchi, or rales noted.
- Rhinitis Control Assessment Test Score: 17.
DISCUSSION QUESTION: What would you recommend and/or prescribe for Brooke’s treatment plan?
ANSWER: After Brooke’s exam, you conclude that her symptoms are consistent with seasonal AR and there is no evidence that supports a diagnosis of sinusitis. You review the Joint Task Force Allergic Rhinitis guidelines:
In 2008, a joint task force (JTF), representing the American Academy of Allergy, Asthma and Immunology; the American College of Allergy, Asthma and Immunology; and the Joint Council of Allergy, Asthma and Immunology developed practice parameters for the diagnosis and treatment of rhinitis.1This evidence-based document provides NPs, PAs, and all medical providers a template by which they can make optimal choices for their patient’s treatment. Nasal corticosteroids are considered to be the most effective medication for controlling AR symptoms and, therefore, are considered first-line treatment for AR.1Nasal antihistamines may also be considered for use as first-line AR treatment.1
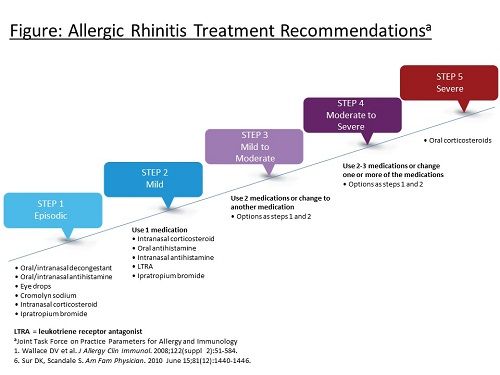
The JTF ascribes to a stepwise approach for AR treatment (see Figure1,6).According to the practice parameters, AR is controlled if nasal symptoms do not interfere with a patient’s normal daily routine and sneezing, nasal itching, congestion, and eye symptoms occur on fewer than 2 days per week. When this is the case, treatment should remain the same or stepped down as defined in the Figure. Alternatively, if a patient has mild interference with activities and is sneezing or has nasal itching, congestion, or eye symptoms 2 to 6 days per week, treatment should be increased by 1 step. If the patient has severe interference with activities and is sneezing or has nasal itching, congestion, or eye symptoms daily, treatment should be increased by 2 steps.1
Patients with moderate to severe persistent AR are considered candidates for immunotherapy if they fail pharmacotherapy and have evidence of specific immunoglobulin-E antibodies to clinically relevant allergens.
The Rhinitis Control Assessment Test (RCAT) was published in 2013 and provides a validated means to subjectively assess a patient’s nasal allergy symptoms. The RCAT is a simple 6-item patient-completed questionnaire designed to reveal any issues of rhinitis symptom control.
The RCAT asks 6 questions:
1. During the past week, how often did you have nasal congestion?
2. During the past week, how often did you sneeze?
3. During the past week, how often did you have watery eyes?
4. During the past week, to what extent did your nasal or other allergy symptoms interfere with your sleep?
5. During the past week, how often did you avoid any activities (eg, visiting a house with a dog or cat, gardening) because of your nasal or other allergy symptoms?
6. During the past week, how well were your allergy symptoms controlled?
RCAT scores range from 6 to 30, with higher scores indicating better rhinitis control. RCAT scores equal to or less than 21 are consistent with patients who have uncontrolled allergy symptoms, and scores greater than 21 are consistent with patients whose symptoms are controlled. When using the RCAT on consecutive visits, a change of at least 3 points is considered clinically meaningful in the context of a patient’s treatment plan. The RCAT can be used to rapidly screen for patients with rhinitis symptom control problems and can help patients communicate with their providers about their symptoms.7
Prior to discussing pharmacotherapy, you review allergen avoidance measures with Brooke and her father, which include minimizing her exposure to spring and fall pollens. Brooke asks your opinion regarding her interest in adopting a cat and you share that because of her atopic history, she would be a great candidate for allergy skin testing to best determine her related risks, if any.
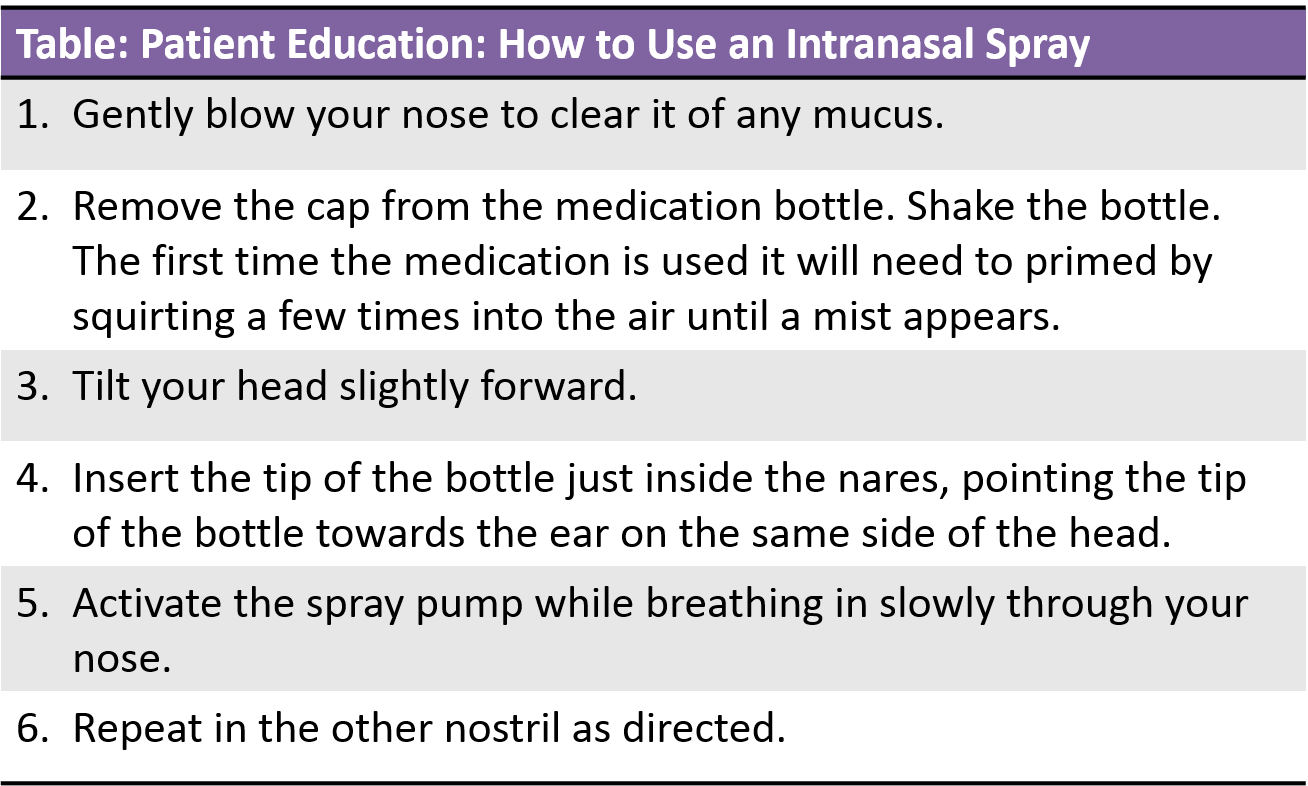
Because Brooke has previously tried and failed treatment with a corticosteroid nasal spray and oral second-generation antihistamine, you decide to step up her treatment by adding an antihistamine nasal spray. Since the publication of JTF’s practice parameters in 2008, a prescription-only combination corticosteroid/ antihistamine nasal spray has become available (fluticasone proprionate / azelastine HCL). Remembering that Brooke complained of her previous nasal spray “running down” the back of her throat, you choose to minimize the volume of nasal spray that she will be taking daily by starting her on the combination corticosteroid/antihistamine spray. The combination product has a quick onset of action that should help her adhere to the treatment plan because she will be able to realize the benefits of the medication in short order. Additionally, the nasal sprays have minimal somnolence adverse effects. Brooke’s father asks you to review the best way for her to take a nasal spray medication and you review the proper steps with both of them (see Table). You discontinue Brooke’s daily use of cetirizine in hopes that any contribution it made to her being sleepy during the school day would stop. You tell Brooke that she can try an alternative second-generation antihistamine (fexofenadine) at bedtime, if needed. You also share with Brooke the benefits of using a nasal rinse, particularly about 20 minutes prior to taking her prescribed nasal spray. You ask Brooke to start taking her allergy eye drops on a consistent daily basis.
Brooke and her father are well pleased with their visit and believe the treatment plan sets them up for success. Brooke is to follow up in 1 month to reassess her symptoms and determine the effectiveness of her treatment plan. You explain to Brooke that she will be asked to complete the RCAT at her next visit to provide a basis for comparison.
Summary
It is widely accepted that the most effective treatment plan for a patient is one that they will follow, is evidence-based, and is created with a patient-centered approach. This case study presents the many aspects of a typical conversation that presents to a retail clinic for a very common diagnosis. Using the JTF’s practice parameters when treating AR while actively listening to the patient will provide a great platform for an effective treatment plan that will optimize the patient’s health outcome.
Karen S. Rance, DNP, RN, CPNP, AE-C, is an allergy, asthma, and immunology specialty nurse practitioner. She is a medical science liaison with Meda Pharmaceuticals and an adjunct faculty member at Indiana Wesleyan University Graduate School of Nursing. Dr. Rance has served on the Board of Directors of the National Association of Certified Asthma Educators and is on the National Heart, Lung, and Blood Institute’s National Asthma Education Prevention Program Expert Panel workgroup. She is the founding chair of the National Association of Pediatric Nurse Practitioners’ (NAPNAP) Asthma and Allergy Special Interest Group and is on NAPNAP’s Clinical Expert Panel for Asthma.
References
- Wallace DV, Dykewicz MS, Bernstein DI, et al. The diagnosis and management of rhinitis: An updated practice parameter. J Allergy Clin Immunol. 2008;122 (2 suppl):S1-S84. doi: 10.1016/j.jaci.2008.06.003. 

- Schappert SM Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007.Vital Health Stat 13. 2011;169:1-38. 

- Marple BF, Fornadley JA, Patel AA, et al. Keys to successful management of patients with allergic rhinitis: focus on patient confidence, compliance, and satisfaction.Otolaryngol Head Neck Surg. 2007;136 (suppl 6):S107-S124. 

- Hoyte FC, Meltzer EO, Ostrom NK, et al. Recommendations for the pharmacologic management of allergic rhinitis.Allergy Asthma Proc. 2014;35(suppl 1):S20-S27. 

- Allergies in America: A Landmark Survey of Nasal Allergy Sufferers.. Mahwah, NJ; HealthSTAR Communications, Inc. www.worldallergy.org/UserFiles/file/Allergies%20in%20America%20(AIA)%20-%20Adult%20Executive%20Summary.pdf.
- Sur DK, Scandale S. Treatment of allergic rhinitis.Am Fam Physician. 2010;81(12):1440-1446.
- Schatz M, Meltzer EO, Nathan R, et al. Psychometric validation of the rhinitis control assessment test: a brief patient-completed instrument for evaluating rhinitis symptom control.Ann Allergy Asthma Immunol. 2010;104(2):118-124. doi: 10.1016/j.anai.2009.11.063.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.





