Prescriptive Authority Update 2017
Nurse practitioners (NPs) and physician assistants (PAs), both rapidly growing professions, stand poised to help alleviate the ever-increasing health care provider shortfall. The NP workforce increased by 75% from 2000 to 2011, and presently, there are 222,000 licensed NPs in the United States.
Nurse practitioners (NPs) and physician assistants (PAs), both rapidly growing professions, stand poised to help alleviate the ever-increasing health care provider shortfall. The NP workforce increased by 75% from 2000 to 2011, and presently, there are 222,000 licensed NPs in the United States.1For PAs, their numbers grew by over 100% from 2000 to 2010, and currently over 115,000 PAs practice in the United States.3
As part of their daily practice, more than 95% of NPs prescribe medications and those working in a full-time practice write an average 23 prescriptions per day. NPs hold prescription privileges in all 50 states and Washington, DC.2PAs also can prescribe medication in all 50 states; Washington, DC; US territories; and the uniformed services.3These privileges, however, vary from state to state, with differing levels of restriction on prescriptive authority as part of a provider’s scope of practice.
CURRENT STATUS OF NP PRESCRIPTIVE AUTHORITY
NPs’ scope of practice includes evaluating patients, diagnosing, ordering and interpreting diagnostic tests, and initiating and managing treatments, which also includes prescribing medications. NPs’ scope of practice is further delineated by the state in which they are employed. The American Association of Nurse Practitioners classifies the NP state practice environment under 3 categories: full practice, reduced practice, and restricted practice.
Twenty-two states and the District of Columbia allow full practice, where NPs generally have the same prescriptive authority as physicians.4For the 16 states categorized as reduced practice, NPs require regulated collaborative agreements with physicians to gain prescriptive privileges, usually with limitations on the medications they are allowed to prescribe. The final and least permissive prescriptive authority category, restricted practice, comprises 12 states. In these states, patient care privileges, including prescriptive authority, likely require physician supervision or delegation.4
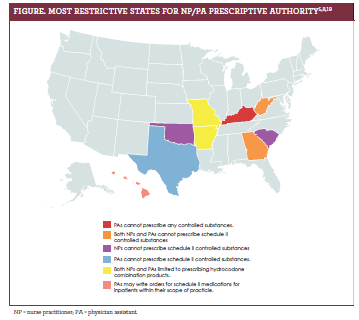
Although all states and Washington, DC, allow NPs to prescribe controlled substances, 6 states have placed additional constraints on the prescription of Schedule II controlled substances. Georgia, Oklahoma, South Carolina, and West Virginia do not allow NPs to prescribe any Schedule II controlled substances; Arkansas and Missouri limit NPs to prescribing hydrocodone combination products only.5
CURRENT STATUS OF PA PRESCRIPTIVE AUTHORITY
A PA’s scope of practice is comparable to an NP's and includes diagnosing, treating, and prescribing as a member of a healthcare team.3All PAs must have a supervising physician, however, and this can be either a doctor of medicine (an MD) or of osteopathic medicine (a DO).6
States vary on the definition of the physician— PA relationship, including how to monitor their interactions.7Every state, except Kentucky, allows PAs to prescribe controlled substances as determined by his or her supervising physician.
Similar to NPs, several states have additional restrictions. Three states—Georgia, West Virginia, and Texas—do not allow PAs to prescribe any Schedule II controlled substances, and 2 states, Missouri and Arkansas, limit PAs to prescribing hydrocodone combination products only. In Hawaii, PAs may only write orders for Schedule II medications for inpatients within their scope of practice (figure5,8,19).8
RECENT PRESCRIPTIVE AUTHORITY LEGISLATION
An analysis of prescriptive authority legislation from 2001 to 2010 reveals NP and PA state regulations have relaxed, giving both more autonomy.9In April 2016, Florida became the most recent state to allow NPs and PAs prescriptive authority for controlled substances when HB 423 was signed into law. This legislation allowed PAs and NPs to begin prescribing controlled substances, including those listed in Schedules II-V, starting January 1, 2017. However, Schedule II medications are limited to a 7-day supply and contain other stipulations, including continuing
education requirements.10
As of this year, many states have legislation in process to expand prescriptive authority for NPs and PAs.11,12 Arizona requires NPs who hold a DEA license to register for its state prescription monitoring program (PMP). In addition, any medical provider contemplating prescribing a controlled substance (specifically an opioid or a benzodiazepine) will be required to check a patient’s controlled substance prescriptions from the previous 12 months through the state’s PMP. This check is required at the time of the initial prescription and at least quarterly thereafter.13
Maine also adopted laws that require providers to check the state’s PMP and that enforce prescribing limits, treatment duration, and mandatory continuing education and electronic prescribing, with some situational exceptions to these laws. New Hampshire and New Mexico enacted laws similar to Maine. In contrast, as of September 1, 2016, Texas passed legislation stating that substance prescribers no longer have to register for their state’s PMP.13
West Virginia expanded prescriptive authority for advanced practice registered nurses (APRNs), including NPs. This new law removes the requirement for physician collaboration related to prescriptive authority once the APRN has completed a 3-year dually documented collaborative relationship with a physician. As a result, APRNs may now write for a 30-day supply of Schedule III medications.13
The American Academy of Physician Assistants (AAPA) will be exploring a new policy through creation of the Joint Task Force on PA Practice Authority. The main objective is to cultivate a plan that removes regulations requiring PAs to have a supervising physician.14A recent survey conducted by the AAPA found 72% of retired and practicing PAs, as well as PA students, support a push for full practice authority (FPA).14
PHYSICIAN OPPOSITION TO NP/ PA PRESCRIPTIVE AUTHORITY EXPANSION
Although there is much support for the expansion of NP and PA prescriptive authority, some physicians oppose regulations that allow NPs and PAs to practice and prescribe without their supervision.15Physicians’ opposing this independence highlight the decreased classroom and clinical education required to become an NP compared with their medical schooling and residency.
They further argue that this creates a 2-tiered health care system and possibly puts patients at unnecessary risk.16
However, while most physicians do not consider NP education to be equivalent to their own, many do appreciate and respect NPs. In 2009, the American College of Physicians published a position paper that recognized the valued part NPs play in the increasing demand for health care.17While the previously referenced AAPA survey found great support for both FPA and expanding prescriptive authority, several comments from respondents expressed concern about potential disapproval from physicians.14Others expressed hesitation about upsetting the existing PA physician relationship.18
CONCLUSION
Staying current on the status of prescriptive authority remains challenging as new laws are introduced and existing laws are updated. Although difficult, it is important to continually monitor and contrast regulations across the United States. Grassroots-level efforts for change can be most effective by coordinating with state-level organizations. Regardless of one’s opinion of prescriptive authority regulations, cooperation among all health care providers is crucial to providing quality patient care and making it available to those who seek it.
Jenna Herman, DNP, APRN, FNPBC, is the FNP program coordinator and an assistant professor at the University of Mary in Bismarck, North Dakota. Her clinical practice includes the emergency department of a level 2 trauma center as well as locum tenens in primary care clinics, nursing homes, and hospitals across rural North Dakota. She is active on the local, state, and national policy
arenas as the AANP North Dakota state representative and an officer of the North Dakota Nurse Practitioner Association in the same role.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.